It’s partly true!……..but it’s not all about sitting. It’s more about how a sedentary lifestyle, including sitting, is perhaps the new smoking. However, unlike smoking which has no health benefits to anyone and I would be happy to eradicate, sitting is something that we don’t want to eradicate and is in fact something that we should have some of, in some capacity. Just not too much!
We know that prolonged sitting is not good for our health, because people have picked up this new message (‘sitting is killing you’) and sales of standing desks have rocketed. Anecdotally however, there are people who also have musculoskeletal problems from standing all day. In short people hear the message that sitting is bad so they stand for long periods instead. It’s important to note prolonged standing can also have adverse health effects. Compared to sitting, when we stand, our hearts and circulatory systems work harder to maintain blood flow to the brain, because they are countering the effects of gravity. Standing still for long periods of time can lead to swelling, heaviness or cramping of the legs. Enforced standing has actually been used as an interrogation technique. That is why sitting is still a part of what we need to do each day but just not in the volume that we do it!
The following is a combination of journal research, blogs, press articles and my thoughts on this topic. I hope you enjoy the read and it creates a call to action for yourself if it’s relevant.
Scary Facts
- Physical inactivity contributes to over three million preventable deaths worldwide each year (that’s 6 per cent of all deaths). It is the fourth leading cause of death due to non-communicable diseases.
- It is also the cause of 21–25 per cent of breast and colon cancers, 27 per cent of diabetes cases, and around 30 per cent of ischaemic heart disease. In fact, physical inactivity is the second highest cause of cancer in Australia, behind tobacco smoking.
- The researchers linked four or more hours a day of television watching with an 80 per cent increased risk of death from heart disease, and a 46 per cent increased risk of death from all causes. That’s compared to people who spent less than two hours a day in front of the box.
So let’s have a look at general activity levels within Australia.
According to ‘Australia’s Health In Brief report 2016’ in 2014–15, almost half (45%) of adults aged 18–64 were inactive or insufficiently active for health benefits, which was similar to the proportion in 2011–12.
In 2009 the “Stand Up Australia” report found:
- 77% of office-based, call centre and retail employee behaviours during their working day was spent sitting (equated to 70% of the day on work days).
- Individuals who spend high amounts of time sitting at work also tend to spend high amounts of time sitting on non-work days. (equated to 62% of the day on non-work days).
- Participants in the study perceived they had much higher levels of physical activity than they did when measured objectively (accelerometers).
- Only 5% of the time on work and non-work days was performing moderate-to-vigorous intensity physical exercise (recommended in the current National Physical Activity Guidelines) with the remainder occupied with light-intensity (incidental) physical activity.
- Significantly more time was spent in light-intensity activity on non-work days compared with work days.
- Interestingly, more moderate-to-vigorous intensity activity occurred on work days compared with non-work days.
If you live a sedentary lifestyle, you have a higher chance of developing:
- Obesity
- Type 2 diabetes
- Heart disease
- Depression and anxiety.
Therefore, living a sedentary lifestyle can be dangerous to your health!
Many people know when they’ve been sitting too long because their back or neck gets sore. These are effects many can relate to because we can actually feel them. But it’s what you can’t feel or see that you may need to be concerned about. Canadian researcher Dr Peter Katzmarzyk, for instance, found that those who sat almost all of the time had nearly a one-third higher risk of early death than those who stood almost all of the time.
University College London researcher Dr Emmanuel Stamatakis found similar results among women in the United Kingdom: those whose work involved mostly standing/walking about had a 32% lower risk of early death than those who worked in sitting jobs.
How does a sedentary lifestyle affect your body?
Humans are built to stand upright. Our heart and cardiovascular system work more effectively this way. Therefore when sitting for long periods of time the following can happen:
Legs and gluteals (bum muscles)
Sitting for long periods can lead to atrophy of large leg and gluteal muscles, where they weaken and waste away. If you don’t use them, you lose them! These large muscles are important for walking and for stabilising you. If these muscles are weak you are more likely to injure yourself from falls, and from strains when you do exercise.
One study reported 2.5 times higher average muscular activity of the thigh when standing compared to sitting. This is important for improving blood sugar profiles and vascular health, reducing the risk of early death.
Weight
Moving your muscles helps your body digest the fats and sugars you eat. If you spend a lot of time sitting, digestion is not as efficient, so you retain those fats and sugars as fat in your body.
The latest research suggests you need 60–75 minutes per day of moderate-intensity activity to combat the dangers of excessive sitting.
Hips and back
Just like your legs and gluteals, your hips and back will not support you as well if you sit for long periods. Sitting causes your hip flexor muscles to shorten, which can lead to problems with your hip joints.
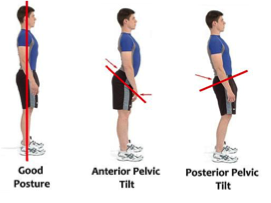
Sitting for long periods can also cause problems with your back, especially if you consistently sit with poor posture or don’t use an ergonomically designed chair or workstation. Poor posture may also cause poor spine health such as compression in the discs in your spine, leading to premature degeneration, which can be very painful.
Anxiety and depression
We don’t understand the links between sitting and mental health as well as we do the links between sitting and physical health yet, but we do know that the risk of both anxiety and depression is higher in people that sit more.
This might be because people who spend a lot of time sitting are missing the positive effects of physical activity and fitness. If so, getting up and moving may help.
Cancer
Emerging studies suggest the dangers of sitting include increasing your chances of developing some types of cancer, including lung, uterine, and colon cancers. The reason behind this is not yet known.
Diabetes
Studies have shown that even five days lying in bed can lead to increased insulin resistance in your body (this will cause your blood sugars to increase above what is healthy). Research suggests that people who spend more time sitting have a 112 per cent higher risk of diabetes.
Varicose veins
Sitting for long periods can lead to varicose veins or spider veins (a smaller version of varicose veins). This is because sitting causes blood to pool in your legs. This is why you here of people getting DVT’s with flying, fluid flows better through a straight pipe than one with a ‘kink’ in it.
Deep vein thrombosis
Sitting for too long can cause deep vein thrombosis (DVT). A deep vein thrombosis is a blood clot that forms in the veins of your leg.
DVT is a serious problem, because if part of a blood clot in the leg vein breaks off and travels, it can cut off the blood flow to other parts of the body, this is a medical emergency that can lead to major complications or even death.
Stiff neck and shoulders
If you spend your time hunched over a computer screen, this can lead to pain and stiffness in your neck and shoulders.
Epidemiological studies show that neck pain is:
- greatest in females
- peaks in the 40’s (although age is not a risk factor, it is a prognostic factor)
- unmodifiable risk factors are;
- female
- previous neck pain
- number of children
- previous LBP
- self-assessed poor health (?modifiable)
- poor psychological health (?modifiable)
- risk factors for office workers are:
- low workplace satisfaction
- keyboard close to the body
- low work variation
- self perceived muscular tension
- not risk factors for office workers:
- frequency of physical activity during leisure
- preventative (risk and prognostic factors) in office workers:
- greater cervical ROM
- greater Cx extensor endurance
- a program of cervical strengthening exercises
How can you save your health from the dangers of sitting?
If you’re not getting enough activity in your day, it’s not too late to turn it around and gain great health benefits in the process.
To obtain the health benefits of standing and reduce the potential adverse effects, the best option is to alternate between sitting and standing. Our message is to stand up, sit less and move more.
Alternating between sitting and standing will increase muscular contractions, stimulating blood flow and resulting in more calories burnt and healthier blood sugar levels. Recent findings from a lab show that alternating between 30 minutes of sitting and standing can improve blood sugar levels after a meal.
The point is that our physical activity guidelines promote breaking up sitting time. We can debate whether standing is better for you than standing but what is most important is that people need to move more. Remaining in one posture for long periods is not good for muscles that are not trained to do that. The other important thing is no matter what you do, there is a difference in doing the right way versus doing it the wrong way and often what we see are the effects of doing it the wrong way.
??Purchase a standing desk??
Now, if you’re leaning towards getting a standing desk but are concerned about your concentration and productivity, there’s some good news. Research shows task performance such as typing, reading and performing cognitive tests is largely unaffected by standing desks. A study by Commissaris et al., (2010) measured both objective and perceived work performance during the performance of five standardised but common office tasks in an office-like laboratory setting. With the exception of high precision mouse tasks, short term work performance was not affected by working on a dynamic or a standing workstation. The participant’s perception of decreased performance might complicate the acceptance of dynamic workstations, although most participants indicate that they would use a dynamic workstation if available at the workplace.
Build more activity into your day
The key is to avoid sitting as much as possible or at least break up your sitting time – even if only by standing, which uses more muscles than sitting. Research shows that people who break up their sedentary time throughout the day, regardless of their total sedentary time, have a better health profile.
Some ways you can incorporate activity into your day are:
- Walk or cycle, and leave the car at home.
- For longer trips, walk or cycle part of the way.
- Use the stairs instead of the lift or escalator, or at least walk up the escalator.
- Get off the bus one stop early and walk the rest of the way.
- Park further away from wherever you’re going and walk the rest of the way.
- Walk to the printer
Be active at work
You can move around at work more than you think:
- Take the stairs instead of the lift.
- Walk over and talk to your colleagues instead of emailing them.
- Take your lunch break away from your desk and enjoy a short walk outside if you can.
- Organise walking or standing meetings.
- Stand up or walk while on the phone
- Stand up every 30 mins
- Try a simple exercise program at work
– forward raise, lateral raise (deltoid) – (use water bottle for weight) 10 X2
– shoulder shrugs 10 X 2
– resisted neck flexion, extension and lateral flexion – 5 sec holds 70-80% MVC
Reduce your sedentary behaviour
Here are some simple ideas to keep moving while you’re at home:
- When you’re tidying up, put items away in small trips rather than taking it all together.
- Set the timer on your television to turn off an hour earlier than usual to remind you to get up and move.
- Walk around when you are on the phone.
- Stand up and do some ironing during your favourite television shows.
- Rather than sitting down to read, listen to recorded books while you walk, clean, or work in the garden.
- Stand on public transport, or get off one stop early and walk to your destination.
And if you work in an office:
- Stand up while you read emails or reports.
- Move your rubbish bin away from your desk so you have to get up to throw anything away.
- Use the speaker phone for conference calls and walk around the room during the calls.
Remember…
Moving around is good for you. It’s good for your physical health as well as your mental health.
Sitting or lying for too long increases your risk of chronic health problems, such as heart disease, diabetes and some cancers.
Being active is not as hard as you think. There are lots of simple ways to include some physical activity in your day.
Consult us at Nelson Bay Physiotherapy & Sports Injury Centre to receive personalised recommendations around your best sitting position, chair set-up, workstation, driving position, computer, keyboard or even standing work-station set-up. We have a range of products to demonstrate and recommend to you to help make your day easier.
Written by: Scott Ward
References:
Andersen L.L., Christensen K. B., Holtermann A., Poulsen O.M., Sjøgaard G., c , Pedersen M. T., & Hansen E.A. (2010). Effect of physical exercise interventions on musculoskeletal pain in all body regions among office workers: A one-year randomized controlled trial. Manual Therapy 15 (2010) 100–104.
Australian Government: Australian Institute of Health & Welfare. Australia’s Health In Brief (2016). https://www.nelsonbayphysiotherapy.com.au/wp-content/uploads/2015/05/Australias-Health-In-Brief-2016.pdf
Commissaris D. A. C. M., Konemann R., Hiemstra-van Mastrigt S., Burford E., Botter J., Douwes M., & Ellegast R. P. (2014). Effects of a standing and three dynamic workstations on computer task performance and cognitive function tests. Applied Ergonomics 45 (2014) 1570e1578
Medibank Private. Stand-up Australia: Sedentary Behaviour in Workers, August 2009. https://www.nelsonbayphysiotherapy.com.au/wp-content/uploads/2015/05/Stand-Up-Australia.pdf
The Sydney Morning Herald http://www.smh.com.au/technology/sci-tech/health-check-sitting-versus-standing-20140818-105jfq.html
Victoria State Government Better Health Channel https://www.betterhealth.vic.gov.au/health/healthyliving/the-dangers-of-sitting



 In the
In the 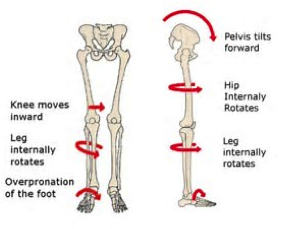
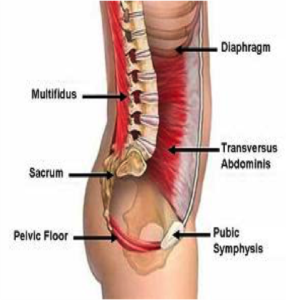
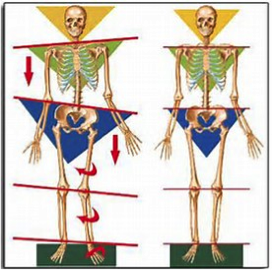
 When your body forgets how to properly activate the gluteal muscles, you lose the ability to move your hips through their full range of motion and compensatory recruitment of other muscles. Ultimately this means that other back and hip muscles tend to tighten up to try and stabilise your wobbly hip. This leads to overactivity of the wrong muscles which alters movement patterns and results in pain and injury.
When your body forgets how to properly activate the gluteal muscles, you lose the ability to move your hips through their full range of motion and compensatory recruitment of other muscles. Ultimately this means that other back and hip muscles tend to tighten up to try and stabilise your wobbly hip. This leads to overactivity of the wrong muscles which alters movement patterns and results in pain and injury.